Next time you pick up a prescription, you could save hundreds of dollars simply by understanding one key difference between medications.
That moment at the pharmacy counter is familiar to many. The pharmacist asks if you want the generic, and a wave of uncertainty follows. Is it truly the same? Will it work as well? This confusion about Generic vs Brand medications leads to a difficult choice: pay more out of fear, or choose the cheaper option and worry. These medication decisions are often clouded by concerns about generic drugs.
You can put those worries to rest. This guide cuts through the noise. We will explain the exact, science-backed differences between generic and brand-name drugs. You will learn how the FDA ensures they work identically in your body. Think of it like a store-brand product different packaging, but the same essential ingredients inside.
We will also provide the latest safety evidence from 2025 research. More importantly, you will get a clear, actionable plan for your next prescription. You will learn the key questions to ask your doctor to make a choice that is right for your health and your wallet. Let’s break down the facts.
1. What Makes Generic and Brand-Name Drugs Different?
Have you ever wondered why a generic drug costs so much less? Is it a completely different medicine? The truth is simpler than you might think. Think of it like choosing between a brand-name cereal and the store brand. The box looks different, but inside, the cereal is nutritionally identical. The same principle applies to your generic drugs and their brand-name counterparts.
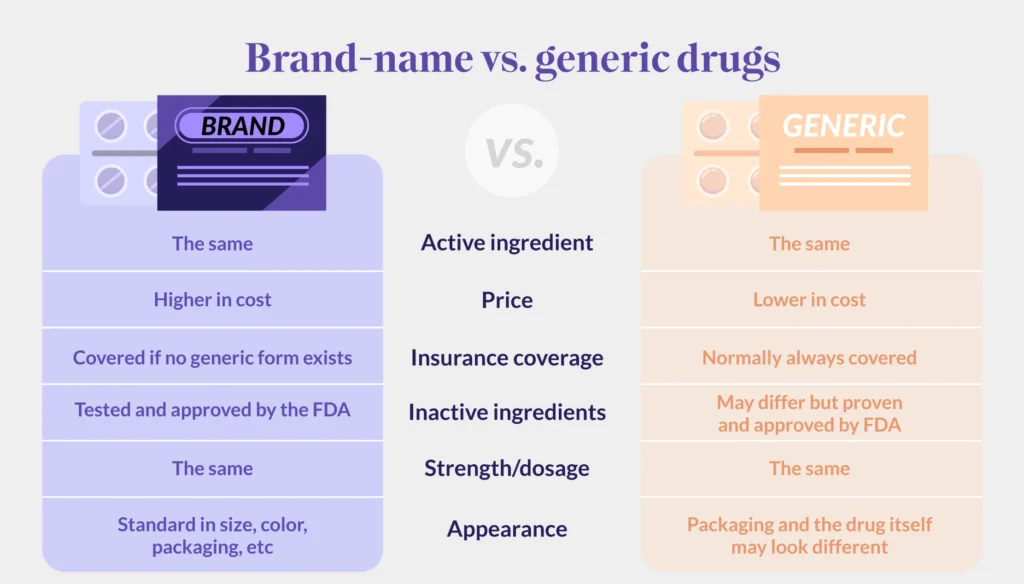
First, and most importantly, both must have the identical active ingredient. This is the part of the medicine that produces the therapeutic effect in your body. Whether it’s for lowering cholesterol or relieving pain, the active ingredient is exactly the same in both versions.
The U.S. Food and Drug Administration (FDA) requires this. A generic must be bioequivalent, meaning it works in the body in the same way and provides the same clinical benefit as the brand-name drug.
The main differences lie in three areas: patents, price, and appearance.

Patents and Development: A brand-name drug company invests heavily in research, development, and clinical trials. To recoup this investment, they are granted patent protection, typically for 20 years. This gives them the exclusive right to sell the drug. Once the patent expires, other manufacturers can produce and sell the generic version.
Brand Name Drug Costs: This is the biggest difference you’ll see. Generic manufacturers don’t repeat those costly clinical trials. They prove their product is bioequivalent to the already-approved brand-name drug. This massive reduction in development cost is why generic drugs cost 80-85% less on average. This is a primary driver behind brand name drug costs.
Inactive Ingredients and Look: The color, shape, and flavoring might be different. These are the “inactive ingredients.” They don’t affect the therapeutic action of the drug. Trademark law doesn’t allow a generic to look exactly like the brand-name product, so their appearance must differ.
The result of these factors is clear. It’s why nine out of ten prescriptions filled in the U.S. today are for generic drugs. Patients get the same medical benefit from the key medication ingredients at a fraction of the price.
2. The Safety and Effectiveness Facts You Need

Are generic drugs truly as safe and effective as their brand-name counterparts? This is the core question for many patients. The answer, backed by rigorous science, is yes.
The foundation of generic drugs safety is FDA approval. For a generic to be approved, it must prove “bioequivalence” to the brand-name drug. This means it delivers the same amount of the active ingredient into your bloodstream in the same amount of time. The medication effectiveness is required to be identical.
You might have heard the FDA allows a 20% variation. This is true, but it’s often misunderstood. In practice, the typical variation observed is only about 4%. More importantly, the brand-name drug has the same allowable variation from one batch to another. Your body cannot tell the difference.
Recent large-scale studies confirm this. A 2025 meta-analysis of 87 studies and over 2.3 million patients found no significant differences in the overall risk of major adverse cardiovascular events between generic and brand-name cardiovascular drugs.

What about inactive ingredients? While these can differ, they rarely cause issues for most patients. In the vast majority of cases, the switch is seamless.
This proven safety record translates into massive savings. Generic medications have saved Americans $2.2 trillion over the last decade. This means you can trust the generic in your hand. It provides the same clinical benefit for a fraction of the cost, making healthcare more affordable for everyone.
3. When Generics Might Not Be the Best Choice

For most people, generic drugs are a perfect choice. But are there times when sticking with a brand name is better? In a few specific situations, the answer can be yes. Understanding these generic medication concerns helps you make a fully informed decision.
The most common issue involves inactive ingredients. While usually harmless, some patients have rare sensitivities to a specific filler, dye, or preservative in a generic version. If you experience a new or different side effect after switching, this could be the cause.
Another key situation involves drugs with a narrow therapeutic index. These are medications where the difference between a helpful dose and a harmful one is very small. For certain thyroid supplements and blood thinners, doctors sometimes prefer to maintain consistency. Switching between manufacturers could potentially cause a slight shift in blood levels that needs monitoring.
When choosing a brand name, it can also come down to simple recognition. Trademark law means generics cannot look identical to the brand. For patients managing multiple pills, a consistent color and shape can prevent confusion and ensure they take the right medication every time.
So, what should you do? The most important step is to talk to your doctor or pharmacist. Don’t just stop taking your medication. Ask: Could my specific condition or prescription be affected by a switch? They can advise if staying with one consistent version is best for your health.
3. Understanding the Real Price Difference

Have you ever wondered why the “sticker price” of a brand-name drug is so high, yet your insurance company pays much less? The reason lies in a hidden system of discounts and rebates that creates a massive gap between the listed price and the final cost. Understanding this is key to seeing the real value of generic medication savings.
Think of it like a high-end grocery item. The brand-name product sits on the shelf with a high price tag. Right next to it is the store-brand version, the generic, with the same core ingredients for a fraction of the cost. The brand-name price covers the store’s marketing and fancy packaging (the drug company’s research and advertising), while the generic only needs to cover the cost of production.
Why Brand-Name Drugs Cost More Initially

Brand-name drug companies invest heavily in research, development, and clinical trials. They also market their products to doctors and consumers. To recoup these massive costs, they are granted a patent, typically for 20 years, which gives them a temporary monopoly. This is why brand name drug costs are high at first. Once the patent expires, other manufacturers can produce the generic version.
How Competition Drives Prices Down
This is where the power of competition kicks in. The FDA has found that when just one generic competitor enters the market, the average price drops by 39%. With a second competitor, prices fall another 15%. When multiple generics are available, prices can plummet by over 95%. This competition is the engine of generic medication savings, making treatments affordable for millions.
The Hidden World of “Gross-to-Net”

But what about the high list prices of brand-name drugs? This is where the “gross-to-net bubble” comes in.
List Price (Gross): This is the manufacturer’s official “sticker price,” known as the Wholesale Acquisition Cost (WAC).
Net Price: This is what the manufacturer actually earns after all rebates and discounts are paid out.
The difference between these two prices is the bubble. In 2024, this gap meant that, on average, brand-name drugs sold for about half of their list price. While list prices grew by only 2.3% in 2024, the actual net prices, after adjusting for inflation, fell for the seventh year in a row.
What This Means for Your Prescription Prices
This system directly impacts your wallet. To control their own costs, most insurance companies strongly prefer generic drugs. Many plans have policies that will only cover the cost of the generic version. If you want the brand-name drug when a generic is available, you may have to pay the full price difference yourself.
The landscape is also starting to shift. In a notable change, some manufacturers are now significantly cutting the list prices of certain drugs. For example, in 2024, manufacturers of widely prescribed insulins slashed their list prices by 50% to 80%. This is a direct effort to pop the gross-to-net bubble and make prescription prices more transparent.
4. Five Questions to Ask Your Doctor or Pharmacist

How can you apply this knowledge to your own healthcare? The answer is simple: have a conversation. Here are five key medication questions to start that discussion and ensure you’re getting the best value.
Is there a generic version of my prescribed medication?
This is your most powerful question. Always ask it for any new prescription or during a medication review. In places like Massachusetts, “generic substitution is required by law unless otherwise specified by the provider.” Your doctor or pharmacist can instantly check for available generic drugs.
Are there any clinical reasons I should stay with the brand-name version?
For the vast majority of people, the answer is no. But it’s always wise to confirm. This question addresses specific concerns, like being on a medication with a narrow therapeutic window. It ensures your safety is the top priority.
How much can I save by switching to the generic?
Make it personal. The answer might surprise you. Most insurance plans now charge significantly higher copays for brand-name drugs. Some may not cover them at all without prior authorization. Your pharmacist can often tell you the exact price difference right at the counter.
Could inactive ingredients in the generic cause issues for me?
This is a smart, proactive question. If you have known allergies or sensitivities (e.g., to certain dyes or fillers), this is the time to mention them. Your pharmacist’s advice is invaluable here, as they have full access to the ingredient lists for both versions.
What should I do if I notice differences after switching?
This final question provides peace of mind. Reassure yourself by knowing the plan. Any unexpected change should be reported to your doctor. In nearly all cases, you won’t notice a difference, but having a plan empowers you.
You are the most important member of your healthcare team. Using these questions turns you from a passive patient into an active, cost-smart partner in your own health. Don’t be shy your doctor and pharmacist are there to help.
Conclusion
The evidence is clear. When it comes to Generic vs Brand Name Medications, generics provide the same clinical benefits at a fraction of the cost. They contain identical active ingredients and meet the same rigorous FDA standards for generic drugs safety. The only significant difference for most people is the price, leading to substantial medication savings.
Think of it like choosing between a national brand and a store-brand at the grocery store. You get the same core product without paying for the fancy packaging and marketing. This simple understanding can save you hundreds of dollars each year.